Targeted Clinical Decision-Making
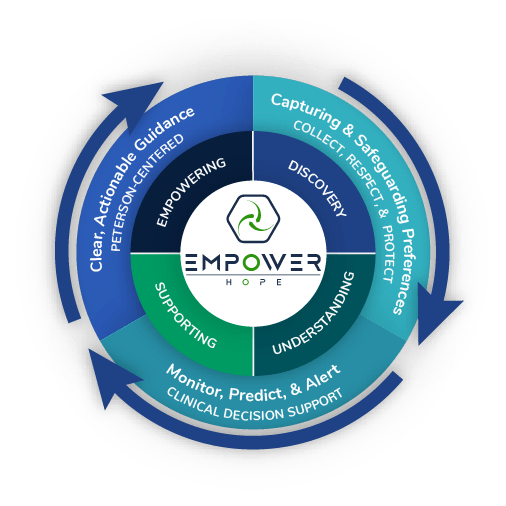
Empower Hope is at the forefront of transforming oncology care by integrating advanced AI-driven mortality prediction models directly into electronic health records (EHRs). Our approach enables healthcare providers to proactively identify high-risk patients, facilitating timely interventions and personalized care plans. By leveraging machine learning algorithms trained on comprehensive EHR data, our system supports clinical decision-making, aiming to improve patient outcomes and optimize resource allocation.
Our innovative methodology, as detailed in U.S. Patent Application US20240257979A1, underscores our dedication to enhancing prognostic accuracy and integrating predictive analytics into everyday clinical workflows. Through this integration, Empower Hope strives to reduce unnecessary interventions, lower healthcare costs, and ensure that patient care aligns with individual values and preferences.
Empower Hope enables patients to forge a personalized path through our complex healthcare system…
Services we offer
1. Digital Advance Care Planning with with engaging media to support high-quality decision making.
a. Advance Directives with electronic signatures and notarization
b. POLST: Portable Medical Orders
c. ePOLST State Registry Vendor
2. Patient Risk Stratification through artificial intelligence.
3. Intervention via strategic integration with EMR, Clinical Decision Support tools, and provider pathways.
4. Advisory services-programmatic, operational, and technical to support goal concordant care and serious illness programs.
5. Speaking engagements regarding Goal Concordant Care, Use of AI in Serious Illness, Palliative Care & Hospice, Advance Care Planning, and more!
Security and Protection for Patient’s Wishes:
Our platform guarantees that patient preferences are respected and safeguarded, providing peace of mind for patients and their families.
Allow every patient throughout their journey to be supported by cutting-edge, evidence-based, operationally endorsed, holistic, patient and family-centered care. Interactive legal Advanced Care Directives and POLSTs integrated into EHRs and IoT.

Visions of the Future
The aging population of the United States is propelling the nation toward a milestone: A historic increase in deaths yearly.
Deaths are projected to reach more than 3.6 million in 2037, 1 million more than in 2015. As the nation’s baby boomer cohort ages (the youngest will be 60 by the end of 2024), the number and percentage of people who die will increase dramatically every year, peaking in 2055 before leveling off gradually.
This creates a crisis for healthcare payors, providers, health systems, and society because:
-
- Patient preferences for end-of-life care are not commonly known, discussed, or actualized
- Significant waste exists in the over 300 billion dollars spent annually in the last 12 months of life
- Most patients have comfort-oriented end of life preferences, and yet too many spend time in the ICU and are hospitalized in the last 6 months of life
- Lack of alignment with patient preferences leads to decreased quality and unwanted care (over and under-utilization)
- The resultant over and under-utilization represents billions of dollars wasted in the US healthcare system annually.

Behind the Tech: Compassionate Artificial Intelligence
We continue to build and introduce new sets of features to push and redefine the boundaries of this self-learning conversational AI solution. With advanced conversation flows that connect the information and self-service solutions, patients need to be increasingly empowered for decision makin.
The system learns and adapts to the patient’s motivations using Empower Hope’s proprietary software, as well as algorithms, statistical models, and automated A/B testing to analyze and draw inferences from patterns in the patient’s data.
Using automation to improve patient outcomes, Empower Hope receives continuous predictive model training to improve their ability to influence patients’ compliance and behaviors using operant conditioning, social learning theory, and other human persuasion techniques.
With all these capabilities, Empower Hope increases capacity and replaces legacy appointment reminders, follow-ups, and collections systems.
Imagine thousands of individual data scientists helping healthcare systems get ahead of the value-based care curve.
Executive Team

Finly Zachariah, MD FAAFP FAAHPM FAMIA
Chief Medical Officer
Dr. Zachariah is recognized as a compassionate and highly skilled supportive medicine physician providing symptom management, pain control, and palliative care for adult and pediatric patients.
He is board certified in Family Medicine, Hospice & Palliative Medicine, and Clinical Informatics. After earning his medical degree from Chicago Medical School, he completed a Family Medicine/Tropical Medicine residency in Whittier at Presbyterian Intercommunity Hospital, followed by a fellowship in Hospice & Palliative Medicine at Kaiser in Los Angeles. Combining his training in tropical medicine with his humanitarian values, Dr. Zachariah has volunteered significant time in underserved parts of the world, teaching palliative care and helping patients in Cameroon, Zambia, India, and Ethiopia.
He also serves as an Associate Chief Medical Information Officer, supporting his colleagues in adopting clinical technologies and refining the Electronic Health Record System to improve care delivery. His programmatic and academic focus includes tailoring patient care to individual values and goals, advance care planning, and leveraging technology to enhance the coordination and delivery of patient-centered medical care in serious illnesses.
He co-founded Empower Hope in 2022 to accelerate the delivery of goal-concordant care for patients with serious illness.

Chris Halsema
Chief Executive Officer
Chris, an Entrepreneur, Engineer, and Data Scientist, became passionate about working with healthcare institutions after seeing the difficulties and costs associated with implementing communication tools.
In 2008, he pivoted his focus from enterprise companies to healthcare, aiming to empower patient-centric solutions that provide the highest level of care and streamline the flow of engagement between patients and their providers.
In 2022, he launched Empower Hope to enhance support throughout a patient’s journey, driving connections and more significant outcomes.
With more than 20 years of experience envisioning and creating integrated solutions in healthcare, fintech, ERP, private cloud, and software development, Chris is recognized for his work and contributions to the early development of Application Service Providers (now commonly known as clouds).
Chris has worked alongside notable companies like IBM and Citrix, and his leadership as CEO of PrudentConnect grew to become one of the first cloud ERP and CRM providers.

Josh Anderson
Chief A.I. Officer
With eight years of professional experience in healthcare technology, I am an area expert in clinical data from EHRs and other sources. My ongoing academic achievements complement this experience with an ever-growing skillset in analytics and data aggregation.
As a Technical Solutions Engineer at Epic, the world’s largest electronic medical record company, I’ve gained experience in soft skills, managing complex projects in various organizational structures, while also honing my technical skills through the development and maintenance of intricate data structures. I am an expert in clinical data structures, both Epic and non-Epic, making me a valuable resource in translating clinical workflows to large aggregated data sets. Amidst the COVID-19 pandemic, I developed a Python script that maps and structures data from organizations across the Epic community, presenting a clean dataset for analysis. As the analytics lead for Cosmos, Epic’s organization-wide research data warehouse, I collaborate with colleagues to identify and clean up incorrectly mapped data. In this role, I also worked with key hospital executives to design and develop data marts that represented diseases with undiscovered pathologies, assisting researchers in drawing new conclusions from the vast amount of medical data now available.

Steven Eskenazi
Business Development SVP
With over 25 years of enterprise healthcare sales experience, I have dedicated my career to driving the growth of early-stage and startup healthcare technology firms. As a sales entrepreneur-in-residence, I specialize in working with disruptive and emerging health-tech companies to establish initial reference customers, generate first revenues, and navigate the complexities of selling to large healthcare organizations.
Recognized for innovation, sales achievements, and revenue growth, I have a proven track record of influencing decision-makers, displacing incumbent vendors, and delivering solutions that improve provider productivity with measurable ROI. My expertise spans national and regional markets, where I have built and led sales teams, shortened sales cycles with compelling value propositions, and helped startups scale in an industry known for its long purchasing processes.
With a deep intellectual curiosity and a results-driven mindset, I bring the professionalism, strategic insight, and ability to challenge conventional thinking needed to drive meaningful change in healthcare technology.
Patent Pending
A method for machine learning-enabled mortality prognosis may include training, based on a set of labeled training samples, a mortality prognosis model to determine a risk of patient mortality within a given timeframe
Publications and Presentations
Prospective comparison of medical oncologists and a machine learning model to predict 3-month mortality in patients with metastatic solid tumors Zachariah, F, Rossi, L, Roberts, L, Bosserman, L
Nudges to improve ambulatory do-not-resuscitate documentation at a comprehensive cancer center Nudges in Healthcare Symposium webinar; May 20, 2021. Roberts L, Zachariah F.